🚨 We have just opened a new study on gastroparesis. You will be paid for your time and travel. 👉 See open study
What is Gastroparesis?
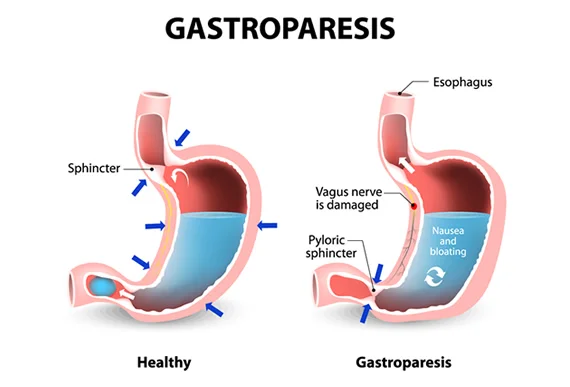
Gastroparesis (Also called delayed gastric emptying) is a long-term (chronic) condition where the stomach cannot empty in the normal way. Food passes through the stomach slower than usual. It’s thought to be the result of a problem with the nerves and muscles that control how the stomach empties.
Is gastroparesis a serious disease?
Gastroparesis is a chronic (long-lasting) condition. This means that treatment usually doesn’t cure the disease, but you can manage it and keep it under control.
Gastroparesis is not usually life-threatening, but complications can be serious. They include malnutrition, dehydration.
Sometimes, more severe complications can occur due to delayed gastric emptying. Individuals can experience obstructions caused by masses of solid hardened food (bezoars).
Gastroparesis life expectancy
Gastroparesis is a serious condition that significantly affects quality of life.
The hope of life of a person suffering from gastroparesis is dependent on the stage of the gastroparesis.
Gastroparesis mortality is highly variable, ranging from 4% in a mixed cohort of inpatients and outpatients followed for 2 years to 37% in diabetic gastroparesis patients requiring nutritional support.
The milder cases have a good expectation of life, but in the more serious cases that it complicates the feeding tube, the life expectancy may be reduced.
However, for many people, gastroparesis is a lifelong condition.
What does Gastroparesis feel like?
Gastroparesis causes a sharp stabbing pain related to intestinal cramps and cramps in the upper part of the stomach caused by the inability to relax and “settle” the food just eaten.
You will feel nauseous or want to vomit, heartburn or reflux, abdominal pain, you will have a feeling of fullness or satiety with small portions of food.
The most common symptoms of Gastroparesis, as we have mentioned, are satiety due to small amounts of food, nausea, vomiting, decreased appetite, abdominal pain, heartburn or gastroesophageal reflux disease (GERD), and regurgitation. These symptoms can lead to weight loss and nutrient deficiencies.
Other symptoms include bloating, muscle weakness, and night sweats. Since the digestive system doesn’t work smoothly, those with the condition also experience periods of low blood sugar while the food remains in the stomach, and high blood sugar when it eventually reaches the intestines.
Why gastroparesis happen?
The exact cause of gastroparesis is not yet known, but it is thought to have something to do with disrupted nerve signals in the stomach. It is believed that the pneumogastric nerve, which controls the movement of food through the digestive tract, becomes damaged and causes food to be digested slowly or not at all.
Other causes of gastroparesis include:
- Viral infections.
- Gastric (abdominal) surgery with injury to the vagus nerve.
- Medications such as narcotics and some antidepressants.
Gastroparesis without a known cause is called idiopathic gastroparesis. Diabetes is the most common known underlying cause of gastroparesis. Diabetes can damage nerves, such as the vagus nerve and special nerves and cells, called pacemaker cells, in the wall of the stomach.
Can gastroparesis go away?
There is currently no cure, but symptoms can be effectively controlled and their progression slowed with appropriate treatment.
One of the best ways to help control the symptoms of gastroparesis is to change your daily eating habits.
Another important factor is the texture of food; liquids and low residue are encouraged (for example, you should eat applesauce instead of whole apples with intact skins).
You should also avoid foods that are high in fat (which can slow down digestion) and fiber (which is difficult to digest).
How Gastroparesis is diagnosed?
A gastroenterologist is the specialist who performs the initial evaluation.
Gastroenterologists use lab tests, upper gastrointestinal (GI) endoscopy, imaging tests, and tests to measure how fast your stomach is emptying its contents to diagnose gastroparesis.
What are the stages of Gastroparesis?
Grade 1, or mild gastroparesis, is characterized by symptoms that come and go and can easily be controlled by dietary modification and by avoiding medications that slow gastric emptying.
Grade 2, or compensated gastroparesis, is characterized by moderately severe symptoms. Individuals with Grade 2 gastroparesis are treated with medications that stimulate gastric emptying and medications that reduce vomiting; such individuals require hospitalization only infrequently.
Grade 3, or gastric failure, is characterized by individuals who do not respond to medications used to treat gastroparesis. These individuals are unable to maintain adequate nutrition or hydration. Required therapies may include intravenous fluids and medications and nutrition or surgery. Individuals with grade 3 gastroparesis often require hospitalization.
Gastroparesis treatment
Treatment of gastroparesis depends on the severity of the person’s symptoms. In most cases, treatment does not cure gastroparesis. Treatment helps people manage the condition so they can be as comfortable and active as possible.
Treatment will focus on treating any underlying problem that is causing it and controlling your symptoms.
Changing eating habits can sometimes help control the severity of gastroparesis symptoms.
Several prescription medications are available to treat gastroparesis, so your doctor may use a combination of medications to find the most effective treatment.
New treatment for gastroparesis?
Currently, INTRALLC is conducting several clinical studies aimed at improving the medical condition of people suffering from gastroparesis. You can view the studies HERE. You will be financially compensated if you qualify.
New treatments are currently being tested, but in order to become available to the general public, clinical studies must first be carried out to prove their effectiveness against the disease.
We have several open studies to test new treatments in search of a cure for gastroparesis and we are enrolling volunteers for it; enrollment includes payment for the time invested in going to the facilities, medicines, among others. If you are interested, you can go to the following link where you can see the open studies and see if you qualify for it.
When gastroparesis get worse?
Gastroparesis symptoms like nausea and vomiting, can worsen with certain factors, particularly when blood sugar control is poor in people with diabetes, or when certain medications are used.
Additionally, conditions like Parkinson’s disease or multiple sclerosis can also affect the nerves controlling stomach motility, potentially worsening symptoms, according to UCLA Medical School.
How gastroparesis affect diabetes
When food that has been delayed in the stomach finally enters the small intestine and is absorbed, blood glucose levels rise.
Gastroparesis can worsen diabetes by making it more difficult to control blood glucose. When food that has been delayed in the stomach finally enters the small intestine and is absorbed, blood glucose levels risGastroparesis makes stomach emptying unpredictable and this can worsen diabetes by making it more difficult to control blood glucose.
Which drugs cause gastroparesis?
Anticholinergics: These medications, used for various purposes, can block nerve signals that stimulate stomach contractions, leading to slower gastric emptying. Examples include atropine, scopolamine, oxybutynin, and benztropine.
Antidepressants: Some tricyclic antidepressants (TCAs) like amitriptyline and nortriptyline, and some selective serotonin reuptake inhibitors (SSRIs) like venlafaxine, can also interfere with the stomach’s ability to empty properly.
Calcium Channel Blockers: These medications, used to treat high blood pressure, can also slow down the stomach’s ability to empty.
GLP-1 Receptor Agonists: These diabetes medications, such as semaglutide, have been linked to delayed gastric emptying and gastroparesis, according to a case report by the National Institutes of Health (NIH) (.gov).
Opioids: These pain relievers, like codeine, hydrocodone, and morphine, are known to slow down stomach emptying and can worsen or even cause gastroparesis.
Other Medications: Nicotine, marijuana, progesterone, and some antipsychotic medications have also been associated with gastroparesis.
Gastroparesis when pregnant
Gastroparesis can cause various complications for both the mother and the fetus, as it can worsen existing gastroparesis or even cause it. Managing gastroparesis during pregnancy requires a comprehensive approach, including dietary changes, medication, and possibly non-pharmacological interventions.
Impact of Pregnancy on Gastroparesis:
- Challenges with management: Treatment options for gastroparesis during pregnancy are limited due to concerns about potential fetal harm from certain medications.
- Exacerbation of symptoms: Pregnancy-related hormonal changes (especially the increase in progesterone) and the expanding uterus can further slow down gastric motility and worsen gastroparesis symptoms.
- Increased risk of complications: Pregnant women with gastroparesis are at higher risk of malnutrition, dehydration, electrolyte imbalances, and potentially preterm labor.
Risks and Complications:
- Diabetic Ketoacidosis (DKA): In women with pre-existing diabetes, gastroparesis can contribute to the development of DKA, which can have serious consequences for both the mother and the fetus.
- Dehydration: Persistent vomiting associated with gastroparesis can lead to dehydration and electrolyte imbalances.
- Malnutrition: Difficulty in digesting and absorbing nutrients can lead to maternal malnutrition, which can negatively impact both the mother and the developing fetus.
- Preeclampsia: Gastroparesis has been linked to an increased risk of preeclampsia, a serious complication of pregnancy.
- Preterm Labor: Nutritional deficiencies and dehydration associated with gastroparesis can increase the risk of preterm labor.
Management of Gastroparesis during Pregnancy:
- Dietary adjustments: Eating smaller, more frequent meals, chewing food thoroughly, and avoiding high-fiber and high-fat foods can help manage symptoms.
- Medications: Certain medications can be used to improve gastric motility, but should be carefully considered due to potential fetal risks.
- Non-Pharmacological Approaches: Lifestyle changes, such as avoiding certain foods and drinks, engaging in light exercise, and seeking stress management techniques, can also be beneficial.
- Multidisciplinary Care: Close collaboration between obstetricians, maternal-fetal medicine specialists, gastroenterologists, and dietitians is crucial for optimal management.
👉 See open studies
The information in this post is for informational purposes only. For medical advice or diagnosis, please consult a professional.
