🚨 We have just opened a new study on gastroparesis. You will be paid for your time and travel. 👉 See open study
What gastroparesis means?
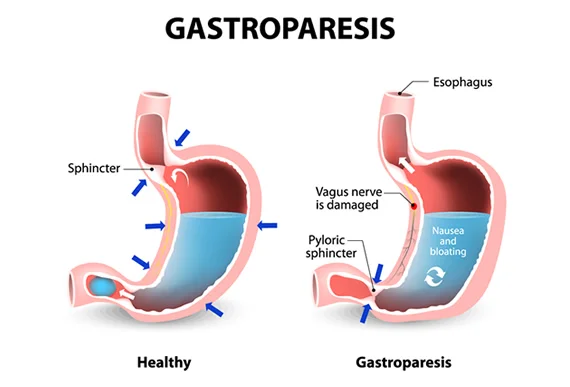
Gastroparesis (Also called delayed gastric emptying) is a long-term (chronic) condition where the stomach cannot empty in the normal way. Food passes through the stomach slower than usual. It’s thought to be the result of a problem with the nerves and muscles that control how the stomach empties.
Is gastroparesis a serious disease?
Gastroparesis is not usually life-threatening, but complications can be serious. They include malnutrition, dehydration, or a bezoar that completely blocks the flow of food out of the stomach.
What are the stages of gastroparesis?
Grade 1, or mild gastroparesis, is characterized by symptoms that come and go and can easily be controlled by dietary modification and by avoiding medications that slow gastric emptying.
Grade 2, or compensated gastroparesis, is characterized by moderately severe symptoms. Individuals with Grade 2 gastroparesis are treated with medications that stimulate gastric emptying and medications that reduce vomiting; such individuals require hospitalization only infrequently.
Grade 3, o insuficiencia gástrica, se caracteriza por individuos que no responden a los medicamentos utilizados para tratar la gastroparesia. Estas personas no pueden mantener una nutrición o hidratación adecuadas. Las terapias requeridas pueden incluir líquidos y medicamentos intravenosos y nutrición o cirugía. Las personas con gastroparesia de grado 3 a menudo requieren hospitalización.
What are the typical symptoms of gastroparesis?
The most common symptoms of gastroparesis include feeling full from small amounts of food, nausea, vomiting, reduced appetite, abdominal pain, heartburn or gastroesophageal reflux disease (GERD), and regurgitation. These symptoms can lead to weight loss and nutrient deficiencies. Other symptoms include bloating, muscle weakness, and night sweats. Since the digestive system doesn’t work smoothly, those with the condition also experience periods of low blood sugar while the food remains in the stomach, and high blood sugar when it eventually reaches the intestines.
Sometimes, more severe complications can occur due to delayed gastric emptying. Individuals can experience obstructions caused by masses of solid hardened food (bezoars).
If excessive vomiting is a symptom, it can cause its own set of complications, including dehydration and malnutrition.
Where is gastroparesis pain located?
Gastroparesis causes a sharp stabbing pain related to intestinal cramps and cramps in the upper part of the stomach caused by the inability to relax and “settle” the food just eaten.
Gastroparesis causes?
The exact cause of gastroparesis is not yet known, but it is thought to have something to do with disrupted nerve signals in the stomach. It is believed that the pneumogastric nerve, which controls the movement of food through the digestive tract, becomes damaged and causes food to be digested slowly or not at all.
Other causes of gastroparesis include:
- Viral infections.
- Gastric (abdominal) surgery with injury to the vagus nerve.
- Medications such as narcotics and some antidepressants.
Gastroparesis without a known cause is called idiopathic gastroparesis. Diabetes is the most common known underlying cause of gastroparesis. Diabetes can damage nerves, such as the vagus nerve and special nerves and cells, called pacemaker cells, in the wall of the stomach.
How Gastroparesis is diagnosed?
Doctors use lab tests, upper gastrointestinal (GI) endoscopy, imaging tests, and tests to measure how fast your stomach is emptying its contents to diagnose gastroparesis.
Who treats gastroparesis
A gastroenterologist is the specialist who performs the initial evaluation.
Gastroparesis treatment
Treatment of gastroparesis depends on the severity of the person’s symptoms. In most cases, treatment does not cure gastroparesis. Treatment helps people manage the condition so they can be as comfortable and active as possible.
Treatment will focus on treating any underlying problem that is causing it and controlling your symptoms.
Changing eating habits can sometimes help control the severity of gastroparesis symptoms.
Several prescription medications are available to treat gastroparesis, so your doctor may use a combination of medications to find the most effective treatment.
Is there any new treatment for gastroparesis?
New treatments are currently being tested, but in order to become available to the general public, clinical studies must first be carried out to prove their effectiveness against the disease.
We have several open studies to test new treatments in search of a cure for gastroparesis and we are enrolling volunteers for it; enrollment includes payment for the time invested in going to the facilities, medicines, among others. If you are interested, you can go to the following link where you can see the open studies and see if you qualify for it.
Can gastroparesis go away?
Gastroparesis is a chronic (long-lasting) condition. This means that treatment usually doesn’t cure the disease, but you can manage it and keep it under control.
One of the best ways to help control the symptoms of gastroparesis is to change your daily eating habits.
Another important factor is the texture of food; liquids and low residue are encouraged (for example, you should eat applesauce instead of whole apples with intact skins).
You should also avoid foods that are high in fat (which can slow down digestion) and fiber (which is difficult to digest).
Gastroparesis life expectancy
Gastroparesis is a serious condition that significantly affects quality of life.
The hope of life of a person suffering from gastroparesis is dependent on the stage of the gastroparesis.
Gastroparesis mortality is highly variable, ranging from 4% in a mixed cohort of inpatients and outpatients followed for 2 years to 37% in diabetic gastroparesis patients requiring nutritional support.
The milder cases have a good expectation of life, but in the more serious cases that it complicates the feeding tube, the life expectancy may be reduced.
However, for many people, gastroparesis is a lifelong condition.
How gastroparesis affect diabetes
When food that has been delayed in the stomach finally enters the small intestine and is absorbed, blood glucose levels rise.
Gastroparesis can worsen diabetes by making it more difficult to control blood glucose. When food that has been delayed in the stomach finally enters the small intestine and is absorbed, blood glucose levels risGastroparesis makes stomach emptying unpredictable and this can worsen diabetes by making it more difficult to control blood glucose.
